ARTICLES > THRIVE
SPECIAL REPORT: CHILDREN AND COELIAC DISEASE
Around 25 per cent of coeliac diseases diagnoses happen in childhood and adolescence. Here's what to expect at different ages and how to support your child.
PRESCHOOL
BIRTH – 5 YEARS
When babies who have been weaned onto solid foods develop coeliac disease, the symptoms can “hit hard and heavy”, explains paediatric gastroenterologist Professor Andrew Day.
“They may have diarrhoea, weight loss, low iron levels, be really grumpy and losing muscle bulk and energy,” he says. “It’s not a pattern that’s expected to occur in a five year old or a teenager.”
Most toddlers and pre-schoolers experience less dramatic symptoms, including diarrhoea, weight loss and bloating, but they can be just as worrying for parents – especially as most children this age haven’t yet mastered the vocabulary to describe how they’re feeling.
Babies and young children are diagnosed with coeliac disease in much the same way as adults, with a blood test and gastroscopy and small intestinal biopsy. What’s different is the responsibility of adjusting to a gluten-free diet rests with the parents, which Prof Day says can help to ease the transition.
“With young children, their food is what you prepare for them, so the environment is a bit more controlled,” he says. “Even when children are at preschool, they won’t necessarily understand why other children will be having foods they can’t have, but over time they will start to learn.”
It’s common for young children to refuse to eat or try new foods, which can be more pronounced among children with coeliac disease, explains Coeliac Australia dietitian Penny Dellsperger.
“Often children have been feeling unwell for some time and they’ve subconsciously realised that it’s food that’s making them feel sick, so to try and introduce new and different foods with different tastes and textures can be really hard,” she says.
Penny says creating a positive environment around the dinner table can help to encourage your child to nibble a carrot or try avocado for the first time. “Ensure you introduce new foods but do so gradually and alongside more familiar things so it’s not too overwhelming for them.”
DID YOU KNOW?
After starting a gluten-free diet, most children with coeliac disease begin to feel better within a few weeks.
CASE STUDY: ELLA, 2
Stephanie Mifsud’s daughter Ella was diagnosed with coeliac disease at 16 months old.
“Ella was very underweight and constantly sick as her immunity was so low,” says Stephanie. “She became lactose intolerant and was having gastro symptoms like vomiting and diarrhoea constantly, which wasn’t helping with her weight. She hadn’t grown since her first birthday. She stopped crawling and could barely lift her head off my shoulder.”
After a frustrating few months visiting different doctors who couldn’t identify the cause of the symptoms, Ella was referred to the Royal Children’s Hospital. “The doctors took one look at her with her clothes off, said they were gravely concerned and ordered more blood tests and urine and stool samples,” Stephanie says.
Several weeks later, Ella’s diagnosis was confirmed. The gluten-free diet led to a huge improvement in her general wellbeing. “She was a completely different child. She had more energy, was playing and crawling again, and was overall happier.”
Now two, Ella is a healthy weight, and the family is adjusting to her diet. “We have found it easy to make swaps at home,” Stephanie says. “And supermarkets have a big variety of gluten-free food available.”
PRIMARY
6-11 years
When a child is diagnosed with coeliac disease, it’s important that parents and siblings are also screened, says Prof Day, as they have a higher risk of also having the condition.
Alongside the more common abdominal pain, “some children will have diarrhoea and a smattering of other symptoms like difficulty gaining weight, mouth ulcers or lethargy,” says Prof Day.
As children start school and gain more independence, planning for birthday parties, sleepovers and school camps can help to make sure your child can enjoy a treat and take part in the fun.
“You’re not there all the time to look after them, so there needs to be good communication with the school about any events that might involve food,” Penny says. “For birthday parties and other occasions at school, giving your child’s teachers a stash of gluten-free snacks is a great strategy.”
Children can start to take more responsibility for their diagnosis and diet. “They can be involved and hear from the dietitian and the doctor about why they need to change their diet,” Prof Day says. “It’s also about adjusting to life with people who are having foods that the child can’t have.”
DID YOU KNOW?
Two-thirds of primary-school-aged children with undiagnosed coeliac disease experience abdominal pain as their main symptom.
CASE STUDY: AIDEN, 9
For Amparo Carillo-Rees, a diagnosis of coeliac disease for her son Aiden was an incredible relief. “Aiden had been struggling for years before being diagnosed,” Amparo says. “We even took a trip to the children’s hospital as he was in extreme stomach pain. When he started school, he had emotional issues every morning, complained of pain in his legs, which would not let him sleep, and was aggressive towards his older brother and us, his parents.”
Aiden was five when he was diagnosed and within months he was “a different child, calm and focused,” Amparo says. “He has thrived at school and in sports and is going well.”
She says the family were all tested for coeliac disease, which revealed that Amparo and her husband both carry a “coeliac gene” but neither the couple nor their other children have developed the condition.
Aiden, who is now nine, is beginning to understand what he can and can’t eat – and asks if he’s unsure. “I know now that when I eat gluten my stomach churns and I feel unwell for days,” Aiden says. “Checking the ingredients before I eat anything from a packet is good, and the gluten-free symbols are helpful.”
SECONDARY
12-17 years
Abdominal pain is a key symptom for teens with coeliac disease. When it comes to diagnosis, Prof Day says a growing number of paediatric gastroenterologists around Australasia now consider what’s called a “biopsy-free pathway”.
“They do the first steps including the blood test, but instead of then doing an endoscopy and looking at the tissue, they do repeat blood tests. Based on abnormalities on those combined blood tests, they conclude that a young person has coeliac disease,” he says. This pathway can only be applied in children and a diagnosis should only be made by a gastroenterologist.
Emerging independence and the influence of peers can have a strong impact on behaviour at this age, which can affect adherence to a gluten-free diet. “A big factor is peer pressure and wanting to fit in with your friends and not appear different,” Prof Day says. “Some young people may push boundaries and go against what they’ve been told to do, especially if they’re diagnosed at an older age.”
Penny says the support of good friends who understand why a gluten-free diet is important can help teenagers combat peer pressure. “If you’re a young person, surrounding yourself with peers that know and understand and support you in following a gluten-free diet can be so, so helpful.”
Parents can help teenagers take greater ownership of the disease by encouraging planning – and the provision of emergency snacks.
“Talk to your young person before they go out – what are their takeaway or other quick options? What snacks can they pack in their bag in case they get stuck?” she says.
“We know that the chips at McDonald’s, for example, are an easy option. There’s always going to be something they can have. It’s important to arm them with information before they head out with friends.”
DID YOU KNOW?
Studies have found children with coeliac disease have a 1.2 to 1.8 times higher risk of depression, mood disorders and behavioural problems.
CASE STUDY: ELIZA, 16
Eliza Hely was diagnosed with coeliac disease when she was seven. Stomach pains, especially during school holidays when her diet was less healthy, were a key sign that something wasn’t right, says her mum Carolyn.
“In the January school holidays she was really, really unwell. She had such bad pain that she couldn’t get off the lounge to travel back to Sydney from Ballina after our holidays.”
Now 16, Eliza has learned how to manage the disease – with the odd slip-up along the way. “When I was 12 or 13, I went to the shopping centre with my friends and everyone was buying these lollies that had gluten and I just ate them,” she confesses. “Then I went to the specialist and lied that I hadn’t been eating gluten.”
These days, she says, sticking to a gluten-free diet is easier because of support from friends.
“If we’re going to dinner, or we’re out and we need to get something to eat, we’ll pick places that have options,” she says. “If I was around people who were always looking for the easiest option, it would be a lot more difficult.”
Travelling overseas is the next challenge. “We have cards from Coeliac Australia to show people but it’s not the same as speaking the language,” Carolyn says.
DID YOU KNOW?
Immediate family members have a 10% increased risk of also having coeliac disease: speak to your GP about family screening.
READ THIS NEXT

INTRODUCING GLUTEN TO YOUR BABY
Should you avoid feeding your baby gluten if there’s coeliac disease in the family? How much gluten is safe? Here’s what you need to consider.

AN AUSSIE TEEN ON GROWING UP GLUTEN FREE
Diagnosed with coeliac disease at seven and now a teen entrepreneur, Isaac Tulemija shares how he handles everything from school to parties.
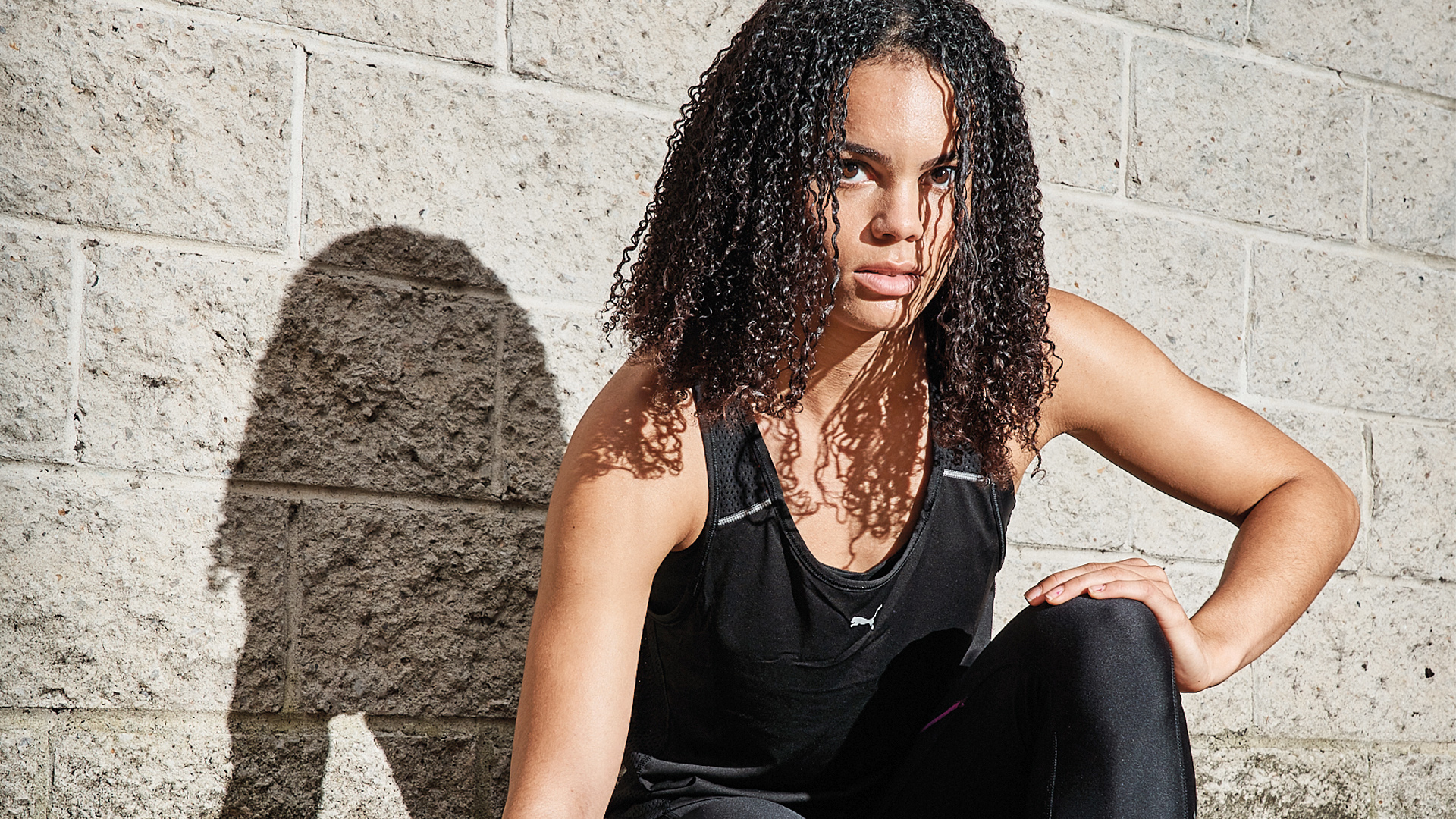
TORRIE’S AT TOP SPEED
Sprint sensation Torrie Lewis happens to have coeliac disease, but her diagnosis has fast tracked her success.
See more















0 Comments